Understanding Diabetic Retinopathy
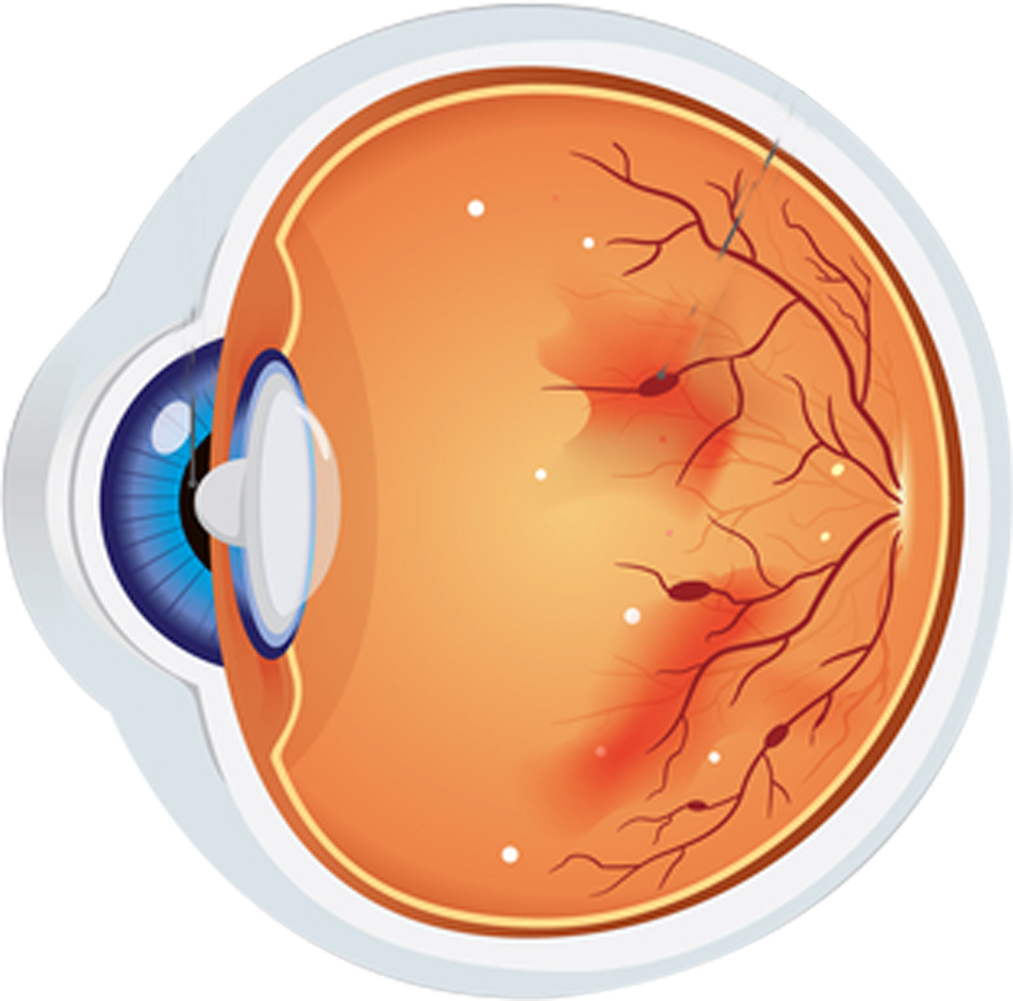
Diabetic retinopathy is a diabetes complication that affects the eyes. It's caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). At first, diabetic retinopathy might cause no symptoms or only mild vision problems. Eventually, it can cause blindness.
The condition can develop in anyone who has type 1 or type 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye complication. Regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.